Diabetic Retinopathy Treatment in The Villages and Ocala, FL
AND HOW DIABETES CAN AFFECT SIGHT: BY THE AMERICAN ACADEMY OF OPHTHALMOLOGY
Diabetes mellitus is a condition which impairs the body's ability to use and store sugar. Elevated blood-sugar levels, excessive thirst and urination, and changes in the body's blood vessels are all characteristics of the disease. Diabetes may affect vision by causing cataracts, glaucoma and, most importantly, damage to blood vessels inside the eye.
What Is Diabetic Retinopathy?
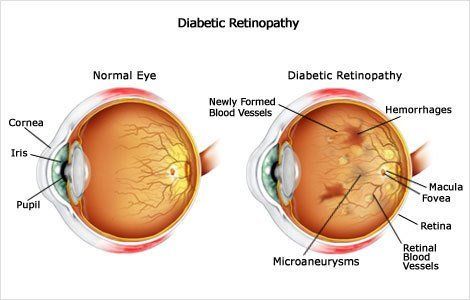
Diabetic retinopathy, a complication of diabetes, is caused by changes in the blood vessels of the retina, the light-sensing nerve layer in the rear of the eye. These damaged blood vessels may leak fluid or blood, and develop fragile brush-like branches and scar tissue. The images that the retina sends to the brain become blurred, distorted, or partially blocked.
The risk of developing diabetic retinopathy increases the longer a person has diabetes. About 80% of the people with at least a 15-year history of diabetes have some blood vessel damage to their retina.
Diabetic retinopathy is particularly likely to occur at a younger age in juvenile diabetics, who have been diagnosed with the condition during their childhood or teenage years. Diabetic retinopathy is the leading cause of new blindness among adults in the United States and people with untreated diabetes are said to be 25 times more prone to blindness than the general population. However, with 'improved methods of diagnosis and treatment only a small percentage of those who develop retinopathy experience serious problems with vision.
Types of Diabetic Retinopathy
Diabetes Can Affect Sight
If you have diabetes mellitus, your body does not use and store sugar properly. High blood sugar levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
Types of Diabetic Retinopathy
There are two types of diabetic retinopathy: non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
NPDR, commonly known as background retinopathy, is an early stage of diabetic retinopathy. In this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates.
Many people with diabetes have mild NPDR, which usually does not affect their vision. When vision is affected it is the result of macular edema, macular ischemia, or both.
- Macular edema is swelling or thickening of the macula, a small area in the center of the retina that allows us to see fine details clearly. The swelling is caused by fluid leaking from retinal blood vessels. It is the most common cause of visual loss in diabetes. Vision loss may be mild to severe, but even in the worst cases, peripheral vision continues to function.
- Macular ischemia occurs when small blood vessels (capillaries) close. Vision blurs because the macula no longer receives sufficient blood supply to work properly.
PDR is present when abnormal new vessels (neovascularization) begin growing on the surface of the retina or optic nerve. The main cause of PDR is the widespread closure of retinal blood vessels, preventing adequate blood flow. The retina responds by growing new blood vessels in an attempt to supply blood to the area where the original vessels closed.
Unfortunately, the new abnormal blood vessels do not resupply the retina with normal blood flow. The new vessels are often accompanied by scar tissue that may cause wrinkling or detachment from the retina.
PDR may cause more severe vision loss than NPDR because it can affect both central and peripheral vision.
Proliferative diabetic retinopathy causes visual loss in the following ways:
Vitreous Hemorrhage: The fragile new vessels may bleed into the vitreous, a clear, gel-like substance that fills the center of the eye. If the vitreous hemorrhage is small, a person might see only a few new, dark floaters. A very large hemorrhage might lock out all vision.
It may take days, months, or even years to reabsorb the blood, depending on the amount of blood present. If the eye does not clear the vitreous blood adequately within a reasonable time, vitrectomy surgery may be recommended.
Vitreous hemorrhage alone does not cause permanent vision loss. When the blood clears, vision may return to its former level unless the macula is damaged.
Traction Retinal Detachment: When PDR is present, scar tissue associated with neovascularization can shrink, wrinkling and pulling the retina from its normal position. Macular wrinkling can cause visual distortion. More severe vision loss can occur if the macula or large areas of the retina are detached.
Neovascular Glaucoma: Occasionally, extensive retinal vessel closure will cause new, abnormal blood vessels to grow on the iris and in the drainage channels in the front of the eye. This can block the normal flow of fluid out of the eye. Pressure in the eye builds up, resulting in neovascular glaucoma, a severe eye disease that causes damage to the optic nerve.

